After completion of this chapter the participant should be able to:
This chapter includes sectiond on:
handwashing
patient isolation
cleaning solutions and
reprocessing single-use devices
Introduction of essential devices to newborn care units is critical to improving newborn survival. However, devices can increase hospital acquired infections if adequate disinfection and cleaning measures are not put into place.
This module focuses on infection control measures associated specifically with the essential devices, staff and visitors. A comprehensive discussion of infection prevention and control measures for a newborn care unit is beyond the scope of this document. Please refer to local and WHO guidelines for more detailed practice guidance.
Hospitals, wards, equipment and staff are all sources of infection for a baby. These infections are called Hospital Acquired Infections (HAI).
HAIs are often caused by bacteria that are resistant to commonly available antibiotics - multidrug resistant bacteria - and are difficult to treat or eradicate from the nursery. Meticulous care is required to prevent infections from spreading from one baby to another in the ward. The prevention and control of all infections include:
Water, Sanitation and Hygiene (WASH) are key elements in preventing and controlling infections.1
Infections are a major cause of morbidity and increased mortality. They often result in prolonged hospital stays and increased costs to the family. Sick and small neonates are at higher risk than other patients of acquiring HAIs due to the number of devices they may come into contact with in neonatal units. Lowering rates of HAIs means less use of antibiotics and ultimately fewer infections with multidrug resistant bacteria which are very difficult to treat in newborns.
While there are a number of critical elements associated with infection prevention and control in newborn units that will be discussed here, the two most important forms of infection control are always hand washing and health screening.
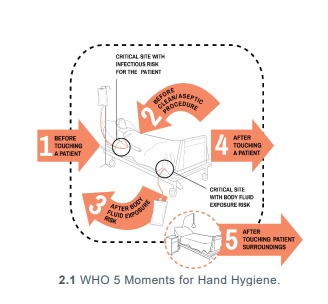
Hand hygiene is the single most important measure to reduce transmitting infections between people and from one site to another on the same patient. All guardians, health care workers (HCWs), or visitors should be taught thorough handwashing (using the WHO technique).
Hand washing or sanitising should be the last thing you do before touching a patient and the first thing you do after completing tasks on a patient
Gloves are worn to protect both HCWs and patients by reducing the spread of infection from bacteria on the hands. Gloves do not change the need to wash or sanitise one’s hands between patient interactions. Gloves should be worn only when necessary and disposed of immediately after use, such as when:
Repeat hand washing or sanitising promptly after removing gloves.
All hospital staff (including HCWs, maintenance and cleaning staff) should wear clean clothes with bare arms below the elbow when entering the neonatal ward. Department policy should be followed; this usually includes that no jewellery (apart from plain wedding bands) is worn, and that nails are kept short, natural, and unvarnished.
Gowns are not a standard precaution for HCWs or families in most neonatal units; if gowns are used, they should not be shared or reused until re-washed.
Any HCW or guardian with an acute or transmissible infection should not be on the ward to minimise the spread of infection. Mothers or guardians who have an acute illness should be isolated with their infants, if possible. Any guardian who has an acute respiratory illness should wear a mask and be especially careful about hand washing.
Departmental isolation policies should cohort at-risk patients with similar infections in an isolation area within the nursery (e.g., babies with multi-drug resistant infections, highly contagious infections, babies born before arrival with signs of infection or any patients with airborne infections). Strict hand hygiene measures should be followed on entry and exit from this area. If equipment is used in any areas where patients are isolated, it should not be returned to the main neonatal care ward until it has been thoroughly cleaned and disinfected according to ward protocol.
Patients should not share cots or radiant warmers. If circumstances mandate that such a practice is unavoidable, cohorting patients with similar illnesses is preferred.
All neonatal medical equipment (suctions, CPAP, vital sign monitors, radiant warmers, etc.) should be cleaned regularly in accordance with the training modules and equipment manuals. WHO recommends 0.5% dilution of chlorine as the standard disinfectant for materials and surfaces contaminated by blood or body fluids.2 For metal and rubber surfaces which may be corroded by chlorine, 70% alcohol is also commonly utilised for low level disinfection. Table 3.1 below provides more information on low-level disinfectants appropriate for neonatal wards.3 Cleaning should be carried out when the equipment power source is switched off and it is unplugged. Care must be taken not to let water or other liquid enter internal to a device. Diluted disinfectants have various lifespans; ward guidelines should include accurate lifespans and dilution schedules for those in standard of practice.
| Disinfectant Common Name |
Recommended Use | User & Equipment Precautions |
| Sodium Hypochlorite, 0.5% or 1% liquid bleach | General disinfectant Kills bacteria, fungi, mycobacteria, spores & viruses Not affected by hard water (e.g., high mineral content water) Use 0.5% concentration for disinfection of surfaces & equipment contaminated with blood and body fluids |
Use in well-ventilated area Respiratory irritant (can cause breathing problems) Appropriate PPE required while handling & using because it can cause skin irritation and burns Should not be mixed with strong acids or ammonia to avoid release of chlorine gas |
|
Alcohol, 70% isopropyl, ethyl alcohol, surgical spirit |
Use on smooth surfaces, table tops, aprons & other small surfaces on which bleach cannot be used (e.g., metal, rubber) Can be used for surfaces including rubber stoppers on medication vials Does not leave residue |
Use in well ventilated area and avoid inhalation Keep away from active heat sources, electrical equipment, flames, hot surfaces. Alcohol must always completely dry on equipment prior to use as otherwise it could result in fire. Allow to dry completely before using area |
Quaternary ammonium compound listed as % concentration of QUAT |
General disinfectant for surfaces/equipment contaminated with blood & body fluids Kills bacteria, fungi and some enveloped viruses (HIV) Has persistent antimicrobial activity when undisturbed |
Use in correct dilution and pour only enough for current use Does not kill spores, TB or non-enveloped viruses Hard water, cotton/gauze, organic matter reduce its effectiveness |
Iodophor |
More commonly used as an antiseptic than a disinfectant |
Causes damage to silicone catheters |
Improved peroxide hydrogen |
General disinfectant for surfaces or equipment contaminated with blood & body fluids Unaffected by organic matter Non-corrosive & safe for workers |
Can be expensive, particularly if purchasing large quantities |
Phenolic germicidal detergent Dettol, Triclosan |
Should not be used in neonatal wards since affordable, effective alternatives are available |
May cause hyperbilirubinemia and/or neurotoxicity in neonates4 |
Bleach is one of the most common substances used to disinfect medical devices. Diluted bleach solutions have a lifespan of 24 hours and should be prepared daily. Possible products are presented in Table 3.2 with appropriate ratios to dilute to a 5% solution.
Product |
% Chlorine Available | Diluting to 5% Solution |
Sodium Hypochlorite |
5.25 – 6.15% |
1-part bleach to 9 parts
clean water |
| Sodium Hypochlorite liquid bleach |
3.5% |
1-part bleach to 6 parts clean water |
NaDCC (Sodium Dichloroisocyanurate) Powder |
60% |
8.5 grams to 1-liter clean
water |
| NaDCC, 1.5 g/tablet tablet | 60% |
6 tablets to 1-liter clean
water |
All horizontal surfaces, including bedside equipment (bed rails, bedside tables, trolleys, commodes, taps, weighing scales, etc.) are cleaned and disinfected with a hospital-approved detergent OR disinfectant such as 0.5% chlorine or 70% alcohol solution at least daily and whenever visibly soiled.
Between patient admissions, all cots and patient beds should be cleaned thoroughly (including all surfaces of incubators) with a hospital-approved detergent/disinfectant such as 0.5% chlorine or 70% alcohol solution.
Floors, surfaces, and handles in the neonatal unit should be cleaned daily with appropriate solutions and according to departmental policy.
To prevent injuries, use extreme caution when handling sharps. This is particularly pertinent whilst drawing blood during glucometer reading.
Place disposable syringes, lancets, needles, and other sharp items promptly in appropriate puncture-resistant containers.
In general, all single use devices should be used as such. However, in resource limited settings consumables meant for one-time use are commonly reused due to cost and supply chain limitations.
Departmental policy for disinfecting and reprocessing single-use-devices must always be strictly followed in order to prevent infection spreading between patients.
When reprocessing single-use devices, it is extremely important that the cleaning process is not delayed following completion of use. There should be a detailed standard of practice as well as oversight processes for ensuring timely and high-quality reprocessing. If equipment is not reprocessed promptly or adequately between patients, it poses a significant infection risk. Please refer to the Reference Manual for Health Care Facilities with Limited Resources Infection Prevention and Control, Module 63 for more detailed guidance on reprocessing of single-use devices.
Respiratory circuits, tubing and equipment are the most commonly reprocessed single-use devices. Syringes, needles, and disposable gloves must never be reprocessed.
| Key Facts for Providers: Infection Prevention |
|