Chronic kidney disease
Definition
Presence of kidney damage or decreased kidney function for three months with implication
for health
- GFR less than 60mL/min or
- Proteinuria, albuminuria, renal tubular disorder or abnormalities detected by imaging
or histology
CKD may lead into problems regarding
- Excretion of urea/ creatinine/waste products
- Electrolyte balance (Na+, K+, Ca2+, PO42-, Mg2+)
- Acid-base homeostasis (HCO3-, H+)
- Maintenance of extracellular fluid volume (and hence blood pressure)
- Promotion of red cell production (via erythropoietin)
- Vitamin D metabolism (and hence bone production)
GFR estimation (eGFR)
eGFR = kx height (cm)/ S-creatinine (mg/dL)
k=0.45 in infants, K=0.55 in children and adolescent girls, k=0.7 in adolescent boys
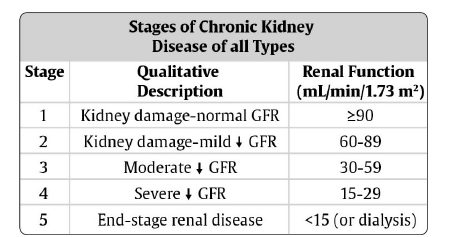
Classification
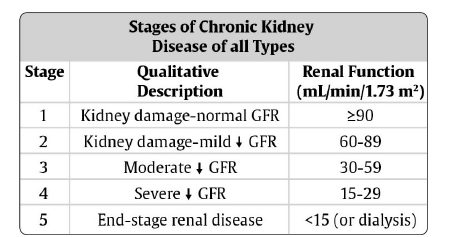
The staging cannot be used for children under two years of age because their normal range
of GFR is lower than in older children.
Causes
- Congenital anomalies
- Obstructive uropathy
- Renal hypoplasia
- Reflux nephropathy
- Polycystic kidney disease
- Glomerular diseases
- Primary glomerulonephritis: Focal segmental glomerulosclerosis (FSGS) is the most
common glomerulonephritis causing CKD
- Secondary causes: HIV nephropathy (stage four disease) and lupus nephritis
- Hemolytic Uremic Syndrome
- Hereditary renal diseases (cystinosis, oxalosis, Alport's syndrome)
- Not resolved Acute Kidney Injury
Important points in history
- Family history of renal disease or hypertension
- Growth history
- Polyuria (congenital anomalies) or hematuria (glomerulonephritis)
- Elevated blood pressure (ask about headaches, seizures, visual disturbance)
- Recurrent urinary tract infections
- Unexplained anemia
- Edema
- Usually the child is asymptomatic until eGFR <30mL/min. Weakness, anorexia,
vomiting, cognitive disturbance are signs of low eGFR
- past medical history of
- Urinary tract infections
- Any serious illnesses
- Family history
Important points on examination
- Nutritional status, height, weight
- Pubertal status
- Blood pressure
- Pallor
- Signs of fluid overload
- Bone deformities (Vit D
- Signs of immunosuppression or multisystem disease (rash, arthritis)
Investigations
- Urine dipstick
- Creatinine, K and Na
- FBC
- Albumin
- HIV-test, hepatitis B and C
- Blood gases (acidosis?)
- Calcium, phosphat, PTH, if possible (private laboratories do)
- Cholesterol levels, if possible
- Renal ultrasound (look for hydronephrosis, structural anomalies, inflammation, renal
size)
- Renal biopsy (very rarely possible)
Complications
- Terminal decline in renal function with profound clinical deterioration
- Anaemia
- Hypertension
- Hyperkalemia
- Fluid overload
- Acidosis
- Mineral and bone disorder
Growth failure, avascular necrosis, skeletal fractures and deformities, andvascular calcifications
- Dyslipidemia
- Left ventricular hypertrophy
- Growth impairment
- Platelet dysfunction - bleeding tendency
- Uremic pericarditis
Treatment
Treat reversible causes
- Obstruction
- Stop nephrotoxic drugs (NSAIDs and tenofovir)
Prevent the progression of kidney disease
Blood pressure
- Salt restriction
- ACE-inhibitors, especially if proteinuria. Consider to stop if eGFR <30mL/min
(risk of hyperkalemia – use only if K and Crea can be monitored regularly)
- Calcium channel blockers (Nifedipine or Amlodipine)
- Diuretics: First line Furosemide. HCT is not effective, if eGFR < 30mL/min.
Avoid spironolactone (hyperkalemia)
- Beta blockers (Atenolol)
Proteinuria
- ACE-inhibitors. See above.
Treat the complications of CKD
Anemia
- Rule out other causes of anemia
- Iron supplements (CKD patients often have iron deficiency)
- Consider Erythropoietin stimulating agents (EPO), if available
- Blood transfusions
Hyperkalemia
- Low potassium diet (avoid bananas, tomatoes, unboiled potatoes (K stays in
potatoes if fried or baked - so boil first), citrus fruits)
- Furosemide
- Resonium (Sodium Polystyrene Sulfonate), if available
Acidosis
- Sodium bicarbonate (or baking soda)
- HCO3 goal is about 20mmol/L
- Treating acidosis may decrease nausea and vomiting
Fluid overload
- Salt restriction
- Furosemide 0.5-2mg/kg
- Hydrochlorothiazide, if eGFR > 30mL/min
Metabolic bone disease (treatment when eGFR < 30ml/min), mostly treatment only
available only in private pharmacies
- Low phosphat diet
- Calciumcarbonate 500mg OD before/during meals to bind dietary phosphat
- Vitamin D (ergocalciferol) 400 IU per day
- If PTH is very high (>5 times upper limit) despite Ca and VitD substitution
- Weight <10kg - 0.05 microgram every other day
- Weight 10-20kg - 0.1-0.15 microgram per day
- Weight 20kg - 0.25 microgram per day
If Dyslipidemia
- Low fat, not long-chain triglycerides, but avoid malnutrition!!
- Statins are not recommended for children under 10 years of age
Nutrition
- Protein restriction is not recommended
- Multivitamin
Psychosocial support, Umodzi involvement
Progression
More rapid if
- Proteinuria
- Hypoalbuminemia
- Elevated blood pressure
- Dyslipidemia
- Anemia
Monitoring and follow-up
- Children with CKD should be regularly checked for growth and well-being, blood
pressure, anemia, and development of bone disease
- Follow up visits in renal clinic
- If CKD stage 4 or 5, refer to palliative care