Oxygen Therapy in Children
Indications
- Airway obstruction
- Cyanosis
- Hypoxia (SaO2 <90%)
- Severe respiratory distress (lower chest wall in-drawing, grunting, head nodding, tracheal tug)
- Tachypnoea
- Shock
- Reduced level of consciousness
- Convulsing
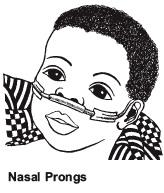
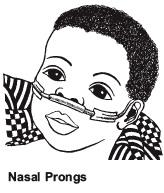
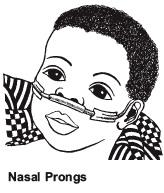
Oxygen delivery
- Nasal prong: Placed just inside the nostrils. Secure with a piece of tape on the cheeks near the nose. Set a flow rate of 1–2 litres/min (0.5 litre/min in young infants) to deliver an inspired oxygen concentration of 30–35%. Humidification is not required with nasal prongs. Care should be taken to keep the nostrils clear of mucus, which could block the flow of oxygen.
- Face mask: can be used if enough concentrators are available – will provide an additional 2-5 litres.
Monitoring
All children receiving oxygen therapy need regular review and observations:
- Oxygen saturations
- Respiratory rate
- Signs of respiratory distress
- Evidence of airway obstruction from mucus or secretions: administer saline drops or gentle suction
- Prong position
- Oxygen concentrator working and correct flow rate
Duration of oxygen therapy
When the child is stable, with minimal evidence of respiratory distress take the child off oxygen for a few minutes. If the SaO2 remains above 90% in room air and there is no increase in respiratory distress, discontinue oxygen. Review the child after 30 minutes and check SaO2 again, to ensure stable.
Care of Oxygen concentrators
Oxygen concentrators need looking after if they are to continue to work for a long time. There are a few simple things that will help:
- If a concentrator is not being used turn it off
- Minimize movement of concentrators
- Take care of the flex (i.e. do not push back against a wall)
- Regularly clean the filter