Pneumonia
Important points in history
- Cough
- Duration(days)
- Associated whooping/vomiting/cyanosis?
- Fever
- Breathlessness – what can they no longer do?
- Eating/ drinking/ feeding
- HIV status
- Immunisation history
- TB contacts
- Prematurity/low birth weight
- Cerebral palsy, other neuromuscular disease
Important points on examination
- ABCs
- Blantyre coma score
- Hydration status
- Head bobbing (in smaller children)
- Grunting
- Nasal flaring
- Tracheal tug
- Lymphadenopathy
- Subcostal and intercostal recessions
- Crackles
- Bronchial breath sounds
- Increased breath sounds (over consolidation)
- Decreased breath sounds (over effusion)
- Reduced air entry/ reduced expansion
- Cyanosis and oxygen saturation
- Finger clubbing
- Tachypnoea (varies by age)
| < 2 months |
> 60 per minute |
| 2-11 months |
> 50 per minute |
| 1-5 years |
> 40 per minute |
Severity
Pneumonia
- Tachypnoea (by age as above)
- Chest indrawing
Severe pneumonia
- Cough or difficulty breathing +
- Central cyanosis / oxygen
saturations <90%
- Severe respiratory distress (e.g.
grunting, severe indrawing, head
bobbing, nasal flaring)
- Convulsions/ LOC/ feeding/ lethargy

- If only cough (+/- fever) and no tachypnoea or indrawing, consider viral URI or differential diagnosis (as listed below)
- It is difficult to tell bacterial / viral pneumonia apart either clinically or radiologically
- Any child who looks toxic should receive antibiotics as this is more likely to be bacterial
Special points if under 2 months old
Investigations
- MPS and PCV
- CXR if not improving or deteriorating
- Gastric aspirate or sputum if suspicion for TB
- Blood culture isn’t usually necessary. Consider if severely unwell, immunocompromised or other signs (eg neck stiffness)
Differential diagnosis of pneumonia
- Foreign body – sudden onset, choking, stridor, focal wheeze
- Pertussis – no or incomplete DPT, “whoops”, well between bouts of cough, no fever
- Tuberculosis – cough ≥2 weeks, weight loss, TB contact, night sweats
- PCP – 2-6 months old, HIV exposed, clear chest, profoundly hypoxic, hyper-
expanded chest
- Other HIV related lung diseases – Kaposi’s sarcoma, lymphocytic interstitial
pneumonitis, chronic lung disease, CMV pneumonitis
- Staphylococcal pneumonia – septic skin pustules. Cavitation on CXR. Consider
flucloxacillin, but ceftriaxone will normally cover
- Severe anaemia – pallor and tachypnoea with a clear chest
- Acidotic breathing - from severe dehydration or local mankhwala
- Cardiac disease – oedema, gallop rhythm, hepatomegaly, clubbed, murmur,
displaced apex
- Paraffin inhalation
- Malaria
- Aspiration – patients with neuromuscular disease/CP, history of vomiting/choking, R
lower lung findings. Consider adding metronidazole or using amoxicillin-clavulanate for po treatment
- Bronchiolitis
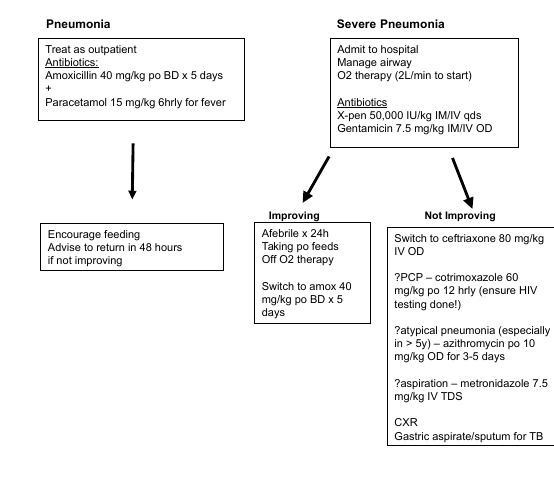
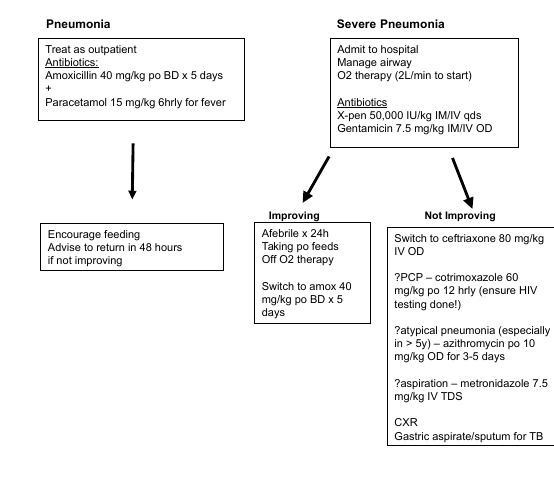
Treatment
See algorithm below
Supportive Care
- Fever (>39 C) causing distress, give paracetamol
- If wheeze is also present, trial of salbutamol nebuliser
- < 4 years - 2.5 mg
- > 4 years 5 mg
- Daily maintenance fluids: oral fluids + feeds (will need more fluids if febrile)
- NGT if child cannot drink/ breast feed
- Viral infections won’t respond to antibiotics. Treat the child, not just the temperature!
If the child looks well, hold your nerve and don’t change the antibiotics. Monitor
closely.
- Oxygen if saturations <90% on room air
- If no pulse oximeter available, give oxygen to patients with increased work of
breathing, any cyanosis, or increased respiratory rate.
Complications of pneumonia
- Effusion/ empyema – stony dull, no air entry. Persistent fever with empyema
(consider TB if you see these on X-ray)
- Pneumothorax – tracheal deviation, hyper-resonance one side
When to discharge
- Eating and drinking
- Not in respiratory distress
- No follow up needed for simple pneumonia