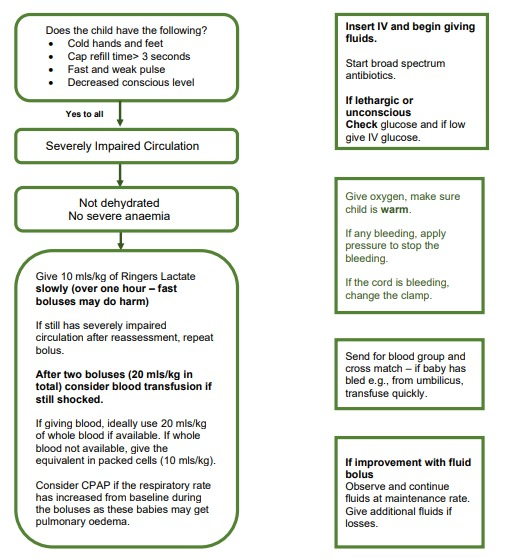
See Overview chart for shock (assessment and treatment)
After completion of this chapter the participant should be able to:
The letters C in ABCCCD
stand for Circulation, Coma and
Convulsions.
This module will help with the systematic assessment, resuscitation and treatment of all NYI
with life-threatening conditions that are most frequently seen in infants less than 2 months of age.
Shock, also called ‘severe impaired circulation’, can be defined as the life-threatening failure of adequate oxygen delivery to the tissues and may be due to decreased blood perfusion of tissues, inadequate blood oxygen saturation, or increased oxygen demand from the tissues that results in decreased end-organ oxygenation and dysfunction. If left untreated, shock results in sustained multiple organ dysfunction, end-organ damage and possible death.
All sick infants are assessed for Airway, Breathing, Circulation, Coma, Convulsions and severe Dehydration (ABCCCD). In view of the poor outcome in many small infants due to co-existent hypothermia and hypoglycaemia, the management of these is detailed here with ABCCCD. Efforts should be made to maintain normal blood glucose and a normal body temperature while managing ABCCCD.
Assess Circulation for Signs of Shock
After the airway and breathing has been assessed, check circulation: Rapid assessment of circulation.
Each of the signs listed above is a sign of impaired (poor) circulation. Severely impaired circulation (shock) is present when 3 of the signs are present
Also important to recognise so that appropriate treatment is given:
Also assess oxygen saturation, heart rate and blood pressure.
Is the Capillary Refill Time (CRT) longer than 3 seconds?
Capillary refill is a simple test that assesses how quickly blood returns to the skin after pressure is applied. It is carried out by applying finger pressure to the centre of the chest over the sternum for 3 seconds. The capillary refill time is the time from release of pressure to complete return of the pink colour. It should be less than 3 seconds. If it is more than 3 seconds the child may be in shock. This sign is reliable except when the room temperature is low, as a cold environment can cause a delayed capillary refill. In such a situation check the pulses and decide about shock.


Is the pulse weak and fast?
Evaluation of pulses is critical to the assessment of systemic perfusion. The radial pulse should be felt. If it is strong and not obviously fast (rate greater than 160 bpm in an infant), the pulse is adequate; no further assessment is needed. In an infant if the radial pulse cannot be felt, palpate for the femoral pulse, if a baby has a weak radial or femoral pulse, it is a worrying sign. Assess hydration status.
Treatment of shock requires teamwork. The following actions need to be started simultaneously.
Giving Fluids for Shock or Impaired Circulation