
Glucose testing on admission to the neonatal unit

Audit data from January 2020 to March 2020


After completion of this chapter the participant should be able to:
5 why analysisapproach and develop action plans.
Sustainable development goal 3.2 aims to reduce preventable neonatal mortality to 12 deaths per 1,000 and under five mortality 25 per 1,000 live births. One strategy that is effective in improving neonatal outcomes is clinical audits including perinatal and neonatal death audits.
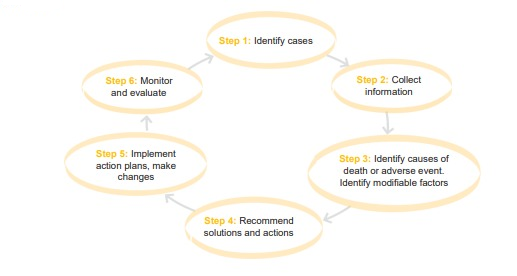
Audits are part of a quality improvement process to enhance patient care and outcomes through systematic review of care against standard criteria. Gaps are identified and appropriate interventions are planned and implemented. Changes are implemented at an individual, team or service level. The assessment is repeated to monitor progress towards the standard of care. Ongoing monitoring and evaluation are used to track improvement in health care delivery and progress towards the goal.
A clinical audit is not research as its purpose is for local use to improve clinical care.
Audits are there to improve bad systems not to find bad people.




Run each Audit Criterion against a selected standard (e.g., WHO or national standards)
| CRITERION | TARGET | EXCEPTIONS | DEFINITIONS and INSTRUCTIONS |
|---|---|---|---|
| All neonates on admission to the sick new born unit must have vital signs documented on admission |
90% | Dead on arrival | Blood glucose |
Conducting the Clinical Audit
The files of patients from the assessment period should be reviewed and required data should be extracted and entered into the data collection form. This will be summarised and analysed in comparison to the required standard. The audit should be done by the team instead of left to one person e.g., the coordinator, so that everyone takes ownership of it.
Example of a data collection tool for blood glucose testing on admission to the SCNU.
| Title – Clinical audit data for neonatal admission assessment | ||||||
| Date of birth |
Sex | Date of admission |
Time of admission |
Time assessed |
Glucose tested Y/N |
Comment |
| 26/02/19 | M | 26/02/20 | 07:30 | 07:30 | N | Glucometer not available |
Once the assessment has been done, the results should be shared with the ward team as well as management. Identify reasons that the standard of care has not been met and agree on strategies on how to address the gaps. E.g., ensuring everyone knows what the standard is, ensuring they have the resources to meet the standard.
Progress on the target can be determined by a repeat of the audit after interventions have been instigated. The time can be agreed on by the team, e.g., reassess progress after 2 months.
| Time period | Target | Achieved | Gaps | Action |
|---|---|---|---|---|
| Jan – Mar | 90% | 40% | Glucometer shared with paediatric ward |
Procure glucometer for new born unit |
| Apr – Jun (Repeat) |
90% | 80% |
Intermediate goals may be agreed upon e.g., improve assessment from 40% to 60% in the next quarter.
Displaying the progress on a graph in the ward can be a way of motivating staff to see how far they have come and the progress towards a goal. A small celebration can be made in the ward upon meeting the standard but remember that the aim is to not only to achieve the standard but to maintain it, so ongoing monitoring and evaluation should be done.
The neonatal death audit process is part of a cycle that aims to improve neonatal outcomes by identifying and reporting neonatal deaths, understanding the trends of mortality and their contributing factors then instigates interventions to address the gaps.
N.B. The aim of a death audit is not to assign blame and witch hunt but rather to identify and address gaps in the system that can contribute to mortality. To facilitate a “no name, no blame, no shame” system names should not be included in the reviewed documents.
Facility audit and review cycle. Page 23; Improving the quality of paediatric care: an operational guide for facility-based audit and review of paediatric mortality. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO.The death audit is a part of a quality improvement process and should be part of an ongoing process.
Conducting death audits should be taken as part of routine care and the ongoing process to optimise the care provided to mothers and neonates in our facilities.
Who should be involved?
The team should be composed of those responsible for caring for the patients on the ward, either in the neonatal unit, the labour ward or theatre and hospital administrators. Senior people within a district facility who can make decisions should participate as without them it may be difficult to make and implement meaningful decisions. The MOHP has agreed on the establishment of Quality Improvement Support Team (QIST) members who are members of the DHMT (District Health Management teams) and a member should be a part of this process
Below is a suggested process of how to carry out a death audit and the team that should be involved:
 Zoom in for details.
Zoom in for details. Planning for the Audit
The neonatal death review form should be filled within 72 hours of a neonatal death by a member of the team managing the patient. This form captures key information regarding the death that may assist in conducting the audit but also captures information without health workers names. These should be compiled in preparation for the neonatal death audit meeting.
Source data for filling this form include the following:
A copy of the neonatal death review form is in the appendix.
Communicate with members of the audit team. If this was not done already, send out minutes and a report of the previous death audit which should include action points. Each facility must agree on the frequency with which they will hold neonatal death audits. This will vary depending on the capacity of the facility but they must be done at least monthly, but some will do this weekly, or fortnightly. Be clear on the period that the audit will cover e.g., 6th to 19th January 2020.
Compile the statistics for the review period including admissions and all the deaths that occurred within the evaluation period. The data required is listed in the neonatal death consolidation form. A specific person must be assigned to do this and will likely need the help of the clerk. To make this process easier, all death files should be kept in one agreed but secure place e.g., a box on the neonatal unit where the ward clerk can easily find them. This will avoid wasting time trying to track down individual file and minimise the list of missing files.
N.B. The team should take note of the quality of data being generated through clinical notes, admission forms and registers. Gaps should be monitored and fed back and action points jointly agreed upon. Poor quality and incomplete data will negatively impact decision making.
Prepare the forms and documentation required for the neonatal death audit meeting.
Aim to start and finish on time so that people become accustomed to the schedule and are more likely to attend. Agree on a secretary and chairperson, these roles should rotate so that everyone takes responsibility.
Key Activities
Identification of Modifiable Factors
Having identified the cause of death, modifiable factors should be identified from the list and categories provided. N.B. there is often more than one modifiable factor for each death.
The list of modifiable factors has two sections, one for the facility where the death occurred and another for the referring facility if relevant. Each section is further categorised into clinical, administrative and caregiver factors.
From the diagram below, one can identify several points at which improvements in care could have reduced the risk of death for the patient.
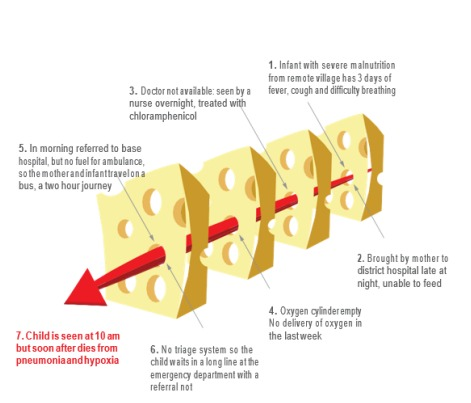
In the meeting, the top 4 or 5 modifiable factors should be identified then a root cause analysis
should be conducted for each. The aim of this approach is to ensure that the actual problem is
identified otherwise interventions implemented will not yield results. Analysis can be done using
the 5 why analysis
.
Once a problem is identified, the reviewers should keep asking “why?” until they arrive at the underlying or root cause of the problem. On average, a root cause is identified after repeating the process 5 times.
Example: Modifiable factor, inadequate monitoring of the patient blood glucose.
Why? They had to borrow a glucometer from the paediatric ward and it was in use.
Why? The ward glucometer is not working.
Why? The batteries are flat.
Why? Batteries were requested but not supplied.
Why? Stores office does not keep that type of battery.
When the team conducting the audit is satisfied that they have identified the problem, action points should be clear, have a responsible person/office assigned to the task and a timeline.
For the example above and possible action point could be:
By the end of .....(date) a sample of the required batteries should be provided to stores by the
nurse in charge so that they can buy the correct batteries.
Summary and Report of the Audit
Information proceeding from the meeting should be summarised in the neonatal death audit consolidation form together with minutes documenting progress on previous action points and the date of the next meeting. These should be circulated to members present and to managers for accountability and follow up of action points. It is helpful for a coordinator or in-charge to brief key management members in person on the audit findings and areas that need their particular support. The next meeting must pick up on the action points to allow continuity and to see the impact of the intervention.
| Key Facts for Providers: Clinical and Death Audits |
|