After completion of this chapter the participant should be able to:
The NYI is most vulnerable to hypothermia during the first few hours after birth, although the condition may occur later too, for example during bathing, on a cold night, or during transportation, if measures to keep the baby warm are inadequate. Sick or low birth weight babies admitted to neonatal units with hypothermia are more likely to die than those admitted with normal temperatures.
Axillary temperature: This method is the routine practice for measuring temperature. It has fewer risks than rectal measurements in terms of injury or infection. Point the tip of the thermometer to the shoulder not the bed to avoid the thermometer reading the air temperature. Record the temperature after the reading has stabilized with a bleep.
Rectal temperature: Do not use this method for routine monitoring. However, it is the best guide for core temperature in cold (hypothermic) sick neonates. Lubricate the thermometer, insert the tip of the thermometer into the rectum not more than an inch. Record the temperature after the reading has stabilized with a bleep.
An easy way to assess a newborn baby’s temperature is by touch
. This can be easily taught to
caregivers. The baby’s abdomen is felt with the back of hand and compared with their own
forehead. Abdominal temperature represents the core temperature and it is reliable in the
diagnosis of hypothermia. Warm and pink feet of the baby indicate that the baby is in thermal
comfort. But when feet are cold and trunk is warm, it indicates that the baby has cold stress.
The NYI has a normal body temperature between 36.5-37.4oC.
| Classification | Mild | Moderate | Severe |
|---|---|---|---|
| Temperature | 36.0-36.4°C | 32.0-35.9°C | < 32°C |
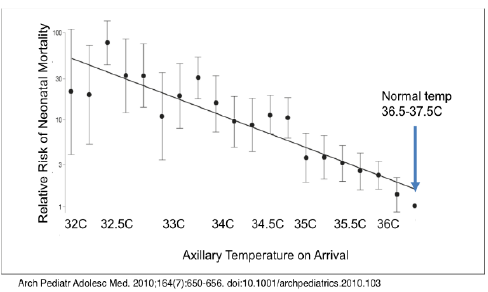
A community-based study has found that mortality increased by approximately 80% for every degree Celsius decrease in first observed axillary temperature, and that relative risk of death ranged from 2 to 30 times for moderate hypothermia, increasing with greater severity of hypothermia (5). A study in India that included only hypothermic babies on admission found mortality ranged from 39.3% for mild hypothermia, 51% for moderate hypothermia to 80% for severe hypothermia. Moderate hypothermia has a much worse outcome when associated with other newborn problems and fatality rates increase to 71% when the baby is also hypoglycaemic, 83% when also hypoxic and 90% when shocked (6).
In Malawi hypothermia has been shown to contribute to mortality in neonates with RDS even when they receive appropriate respiratory support such as oxygen or bCPAP. None of the neonates who had an average temperature of less than 35.8oC survived to discharge. Correction of the hypothermia resulted in improved outcomes and benefit from bCPAP – in this cohort all 30 neonates for whose temperature readings were more than 35.8oC more than half the time survived regardless of their initial temperature.
Newborn baby’s temperature falls within seconds of being born and sick NYI are often hypothermic. If the temperature continues to fall the baby will become sick and may even die.
| Method of Heat Loss | Prevention |
|---|---|
| 1. Evaporation (e.g., wet baby) | Immediately after birth dry baby with a clean, prewarmed, dry cloth and then wrap in another dry warm cloth. |
| 2. Conduction (e.g., contact with a cold surface of a weighing scale) | Put the baby on the mother’s abdomen for the first 30 min or on a warm surface, delay weighing if room too cold. Place a light, dry material in the weighing scale and zero the scale. |
| 3. Convection (e.g., exposure to draught) | Close the windows, switch off fans and air conditioners and, if circumstances permit, wait for the room to warm up to 25ºC before performing a Caesarean section. |
| 4. Radiation (e.g., cold surroundings) | Provide a warm, draught free room for delivery or neonatal ward; at least 25ºC. |
These are procedures to be taken at birth and during the next few hours and days in order to minimize heat loss in all newborns.
If there are no signs of distress, a mother can provide a warm environment with skin to skin contact for the baby. If the baby is <2500 grams this should be continued as KMC. Place the baby, with a nappy and hat, upright inside mother’s clothing against mother’s bare skin over the chest. A loose blouse, sweater, or wrap tied at the waist holds the baby. The baby should wear a hat. Let baby suckle at the breast as often as s/he wants, but at least every 2 hours. See also KMC
Bathing should be delayed until at least 24 hours after birth. Blood, meconium, and some of the vernix will have been wiped off during drying at birth. The remaining vernix does not need to be removed as it is harmless, may reduce heat loss and is reabsorbed through the skin during the first days of life.
Weighing the baby at birth puts him/her at risk of heat loss and should be postponed for at least two hours unless the room temperature is warm.
As a rule, newborns need one or two more layers of clothing and bedding than adults. Covers should not be tight to allow air spaces between the layers as trapped air is a very efficient insulator. Keep ambient atmospheric temperature warm for baby’s weight and postnatal age. Monitor body temperature 4 hourly.
If a baby cannot stay with their mother for KMC, then a hot-cot is helpful. The Blantyre hot-cot is a simple incubator that uses four 60-watt light bulbs to raise the air temperature within the cot by 1.5°C per light bulb. A baby may need one, two, three or all four bulbs to be on to stay warm. Check the baby’s temperature after an hour in the cot, and if the baby’s temperature increases, turn off two bulbs to avoid overheating the baby and recheck the baby’s temperature regularly. It may be warm enough just to have one bulb, or no bulb on and the Perspex lid raised.
The body cannot function well when it is cold. There may be:
The NYI should be re-warmed carefully and gradually to prevent seizures, the temperature needs to rise by 0.5oC per hour. The method selected for re-warming will depend on how sick the NYI is and availability of mother, staff and equipment.
The methods to use include:
Radiant warmers may be used on any neonatal patient admitted to the nursery ward, but especially for: