E 9 Glucometer
This equipment is important for Hypoglycaemia and Hyperglycaemia as decribed in
How to Manage Hypoglycaemia or
Hyperglycaemia in NYI.
Subsection of this chapter:
- Clinical Problem
- Assessment
- Management
- Infection Prevention
- Complications
- Care & Maintenance
- Troubleshooting & Repair
NEST360°. Newborn Essential Solutions and Technologies-Education – Clinical Modules:
Glucometer. (June 2020). License: CC BY-NC-SA 4.0.
Clinical Problem
Assessment of blood glucose with a glucometer should be conducted as part of
routine assessment for all infants on admission.
Glucometers should also be used during continuing management for all sick or at-risk
patients. Hypoglycaemia may present as:1
- Jitteriness
- Irritability
- Hypotonia
- Lethargy
- Reduced level of consciousness
- Failure to feed or poor feeding
- Seizures
- Hypothermia
- Apnoea
or irregular breathing
Hypoglycaemia may also be asymptomatic or the signs may be very non-specific and
identified incidentally as part of routine blood glucose testing.1
It is important to identify
hypoglycaemia as it may lead to permanent brain damage. Prematurity, intrauterine
growth retardation, birth asphyxia, babies born to diabetic mothers, and sick babies are
all especially prone to develop hypoglycaemia.
Assessment
Hypoglycaemia occurs in 10% of healthy neonates but can also directly contribute
to both morbidity and mortality.2,3 It is the most common medical emergency to
occur in neonatal patients.
Glucometers (2.1) provide a rapid measurement of approximate whole blood glucose
level1
to direct treatment for patients with mild to severe hypoglycaemia. Where available,
point of care tests should be confirmed by laboratory analysis when hypoglycaemia is
persistent, recurrent, or there is concern about accuracy of the point of care device.

Glucometers use test strips (2.2) with a glucose oxidase electrode. These strips generate
a current proportional to the glucose in the blood that reacts with the glucose oxidase,
which is then measured and analysed to determine an estimated blood glucose level.

There are multiple types of glucometers, including portable and benchtop. Glucose strips
that change colour according to a visual scale are also available for measuring glucose
levels. These are not recommended due to their higher inaccuracy and subjective
nature of measurement. Not all glucometers are accurately able to measure
hypoglycaemia in neonatal patients;4,5 all devices in use should be thoroughly validated
for use both in neonatal patients and as an assessment of hypoglycaemia.
Glucose levels in all neonatal patients should not fall below 2.5 mmol/L
(45 mg/dL).
Management
Management of a glucometer covers how to use the device in a variety of settings,
including set up for a patient, patient preparation & conducting & concluding the
assessment.
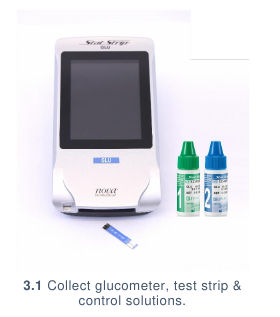
SETTING UP FOR A PATIENT
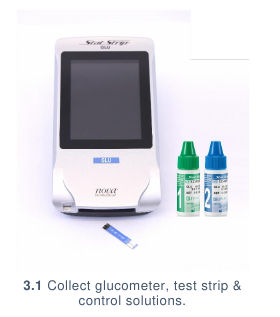
- Collect: (3.1)
- Glucometer
- Glucometer strips
- Control solutions
- Turn on the glucometer. This may be completed by pressing the power button of
the glucometer or inserting a glucometer strip into the glucometer strip port.

- Fully insert a test strip into the meter. (3.2) The strip should click into place.
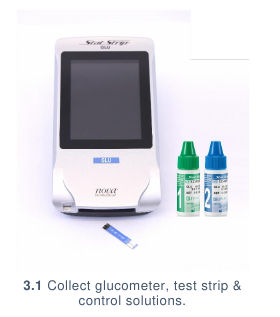
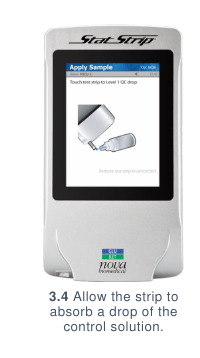
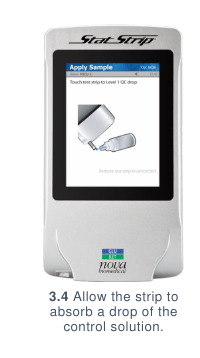
- A Quality Control test should be conducted daily. If this has not been completed,
perform a test using the control solutions provided with the glucometer (3.3), or a
solution of known glucose content. The solution should be placed on the strip as
with a normal sample. (3.4) The results should appear within seconds as a Pass.
(3.5)


PREPARING A PATIENT
- Assess patient for clinical conditions associated with hypoglycaemia.
- Always explain the purpose, risks and benefits of a procedure to guardians BEFORE
performing the procedure.
- Follow handwashing protocol and put on gloves.
- Collect:
- Gloves
- 70% Alcohol
- Cotton swab
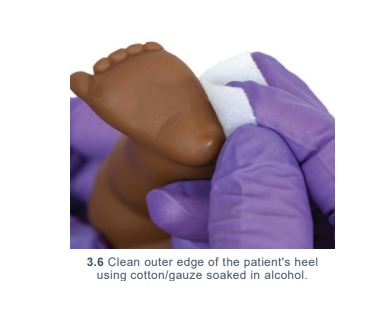
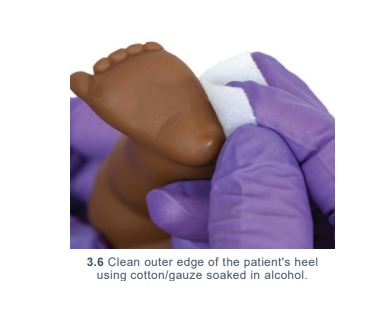
- Clean the skin on the outer edge of the patient’s heel using cotton wool soaked in alcohol.
(3.6) Allow the alcohol to dry before testing. Blood glucose samples should never be
taken from the finger of a neonate. Avoid areas of skin which are poorly perfused,
oedematous, inflamed or infected.
ASSESSING A PATIENT
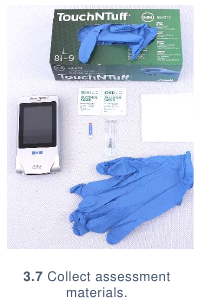
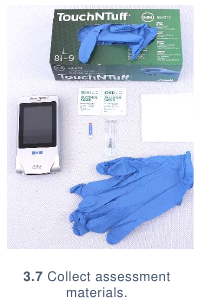
- Collect: (3.7)
- New lancet
- Glucometer
- Glucometer strip
- Cotton swabs
- Alcohol (swabs/solution)
- Gloves
- A small tray to carry the items above
- Follow handwashing procedures & put on gloves.
- Insert glucometer strip into glucometer and ensure it is turned on.
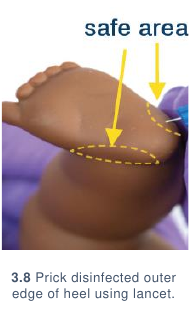
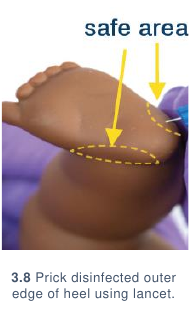
- Using the lancet, prick the disinfected outer edge of the heel. (3.8) A blood drop should
form. If this does not occur, massage the heel to generate the blood drop. The patient may
cry during blood collection as use of the lancet can be painful.
- Wipe the first drop from the patient’s skin and generate an additional blood drop. Collect
the second blood drop on the tip of the glucometer strip. (3.9) The glucometer should
automatically absorb the blood drop.

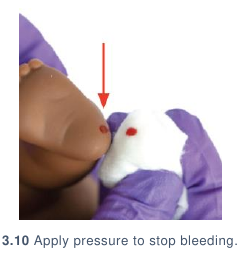
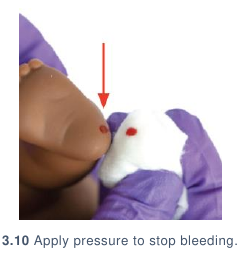
- Using a dry cotton swab, apply pressure to the heel to stop the bleeding. (3.10)
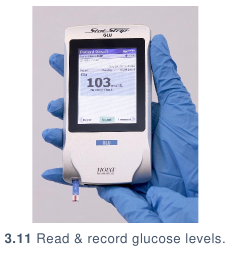
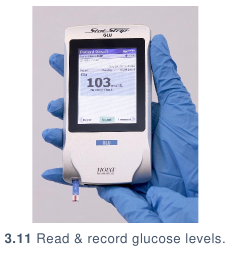
- Blood glucose level will be displayed as a number on the glucometer screen. (3.11) Read
and record the glucose levels. If the measurement is not in accord with the clinical
condition of the patient, repeat the test.
- Compare glucose levels to normal standards.6
CAVE - this is the NEST recommendation. Find the COIN recommendation:
here
- If levels fall below 2.5 mmol/L (45mg/dL) but the baby is alert, can breastfeed, be
fed by cup and spoon or has a nasogastric tube, give extra feed and recheck in 2
hours.
- If levels fall below 2.5 mmol/L (45mg/dL) but the baby is unable to feed,
immediately administer 2 mL/kilogram 10% dextrose IV and then start an infusion
of 10% dextrose.
- If levels fall below 1.2 mmol/L (21.6mg/dL) in any baby, immediately administer
2 mL/kilogram 10% dextrose IV and then start an infusion of 10% dextrose.
Whenever hypoglycaemia is found and treated, the blood glucose should be rechecked 30
minutes after intervening.
| ? |
ALERT 3.1: Variance in international standards for
hypoglycaemia management |
| American Academy of Pediatrics, Pediatric Endocrine Society and WHO
are all in agreement that glucose levels below 2.5mmol/L (45mg/dL)
signify hypoglycaemia in newborns. However, they differ on the specific
actions that should be taken and how aggressively to manage glucose
levels below 45mg/dL, (2.5 mmol/L). For a full discussion of management
of hypoglycaemia in newborns, these documents should be referenced
and local practices put into place.7–9 |
CONCLUDING ASSESSMENT
Remove the glucose strip from the glucometer and dispose of strip in hazardous waste
container. Dispose of the used lancet in sharps container. Remove gloves, dispose in
hazardous waste container, and wash hands.
Infection Prevention
Routine and adequate cleaning of medical devices is critical to prevent hospital-acquired infections in newborn care units. If devices and equipment are not
disinfected or reprocessed promptly or adequately between patients, they may
pose a significant infection risk.
GENERAL INFECTION PREVENTION
- Clean hands with soap and water or alcohol before and after assessing a patient
using a glucometer or handling any materials that will be used on a patient (e.g., a
lancet). Gloves should be worn throughout the process of taking a blood
glucose measurement and disposed of immediately after concluding the
measurement.
- Always thoroughly clean the patient’s skin before taking a measurement using a
glucometer. Inadequate cleaning of the skin may result in an infection. Taking a
sample from a site with a skin infection also poses the risk of infection
dissemination.
- Ensure that all patient-related consumables are new before use. Materials used in
blood glucose measurements should never be reused.
- All patient-related consumables should be stored in a clean, dry location.
Glucometer measurement strips should be stored in an airtight container and
according to hospital policy.
- Follow universal precautions of handling sharps.
| ? |
ALERT 4.1 Equipment Disinfection |
| Disinfection of equipment should always comply with manufacturer
guidelines. General guidance on environmental cleaning and disinfection
of equipment was taken from the Infection Prevention and Control:
Reference Manual for Health Care Facilities with Limited Resources,
Jhpiego, Module 68 which lists isopropyl alcohol (70-90%), sodium
hypochlorite (0.05% or >100ppm available chlorine) quaternary
ammonium, and Iodophor germicidal detergent as appropriate for low
level disinfection. Phenolic germicidal detergent is also listed in this
category but should not be used in neonatal wards since affordable,
effective alternatives are available; and, there are concerns it may cause
hyperbilirubinemia and/or neurotoxicity in neonates.9
When utilizing re-processed devices meant for single-use (like
temperature probes), careful attention must always be paid to assure that
devices are continuing to function properly.
|
DISINFECTION AFTER USE
- Remove the glucose strip from the glucometer and dispose of strip in hazardous
waste container. Dispose of used lancet in sharps container. Remove gloves,
dispose in hazardous waste container, and wash hands.
- Wipe down the glucometer with 70% alcohol. (4.1) Be careful not to submerge or
drip alcohol onto the glucometer, particularly in its glucometer strip reading slot.

Complications
Introduction of equipment in newborn care units poses clinical and device
complications for patients. Awareness of potential complications is critical to
maximise patient safety.
CLINICAL COMPLICATIONS
- Bruising: inappropriate or repeated attempts to collect blood for glucose testing may
result in bruising to the heel.
- Bleeding: if pressure is not applied post blood collection bleeding may persist for a short
period of time. Continued bleeding may indicate an underlying bleeding disorder.
- Artery, nerve or bone damage: do not use the back or the inner part of the heel for blood
collection. This may cause artery, nerve, or bone damage.
- Pain: the lancet prick can cause pain, employ appropriate soothing measures.
- Infection: rarely infection may occur at the site if infection precautions are not adequate.
DEVICE COMPLICATIONS
- Falsely high readings: dextrose gel or substances on the skin can affect readings. If you
record a very high reading in a patient that is otherwise showing symptoms of
hypoglycaemia, consider recleaning the patient’s skin and retaking the measurement.
- Expired glucose strips: outdated or improperly stored glucose strips can produce
inaccurate readings. Make sure the lid is kept tightly on the strip container as humidity
damages the strips. When possible, unexpired glucometer strips should not be used.
Care & Maintenance
Users are responsible for basic first-line care and maintenance to ensure
equipment lasts to their potential lifetime.
POWER SOURCE
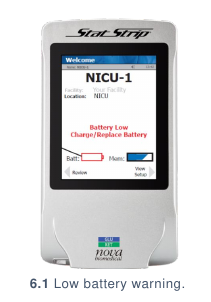
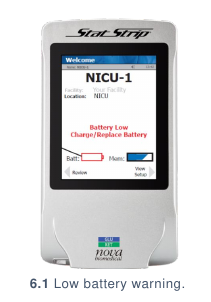
A glucometer is powered by replaceable or rechargeable (6.1) batteries. If using a
rechargeable device, the users should regularly charge the pulse oximeter when not in
use to ensure power in the event of a power outage.
WARD LOCATION
The glucometer and associated glucometer testing strips should be stored in a clean, dry
and secure area. As glucometers are fairly small, care should be taken to ensure that
they remain on the ward and accessible for use when required. If the glucometer has a
docking or charging station, it should be kept on the dock or charging station when not in
use. (6.2)

USER PREVENTIVE MAINTENANCE
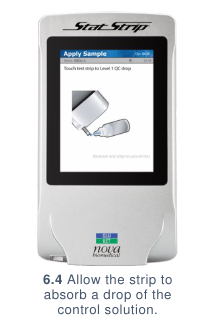
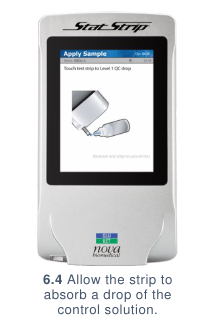
Glucometers require little preventive maintenance beyond recharging or replacing
batteries. A Quality Control test using the control solutions provided with the glucometer
(6.3), or a solution of known glucose content should be conducted monthly or when
changing glucometer strip containers to ensure consistent results. The solution should be
placed on the strip as with a normal sample. (6.4) The results should appear within
seconds as a Pass. (6.5)


Troubleshooting & Repair
Although users are not responsible for repairing their devices, there are steps that
may be taken to troubleshoot first-line errors that may occur before contacting
maintenance or engineering support.
| 1 |
The glucometer is not turning on |
|
- Some models of glucometer require a strip to be inserted and will automatically
turn on once this is completed. Try inserting a glucometer strip.
- If the glucometer still does not turn on, try charging or replacing the batteries. If
the glucometer still does not turn on, contact your maintenance department.
|
| 2 |
The glucometer is providing results consistently incompatible with patient
conditions: |
|
- Check the expiration date of the glucometer strips. If the strips are expired, try
using non-expired strips.
- If the results are still inconsistent, complete a quality control test as described
in Glucometer: Care & Maintenance | Preventive Maintenance If the results
are still inconsistent, contact your maintenance department.
|
References
- Thompson-Branch, A. & Havranek, T. Neonatal Hypoglycemia. Pediatr Rev 38, 147–157 (2017).
- Samayam, P. Study of Asymptomatic Hypoglycemia in Full Term Exclusively Breastfed Neonates
in First 48 Hours of Life. Journal of Clinical and Diagnostic Research. 9, 4 (2015).
- Heck, L. J. & Erenberg, A. Serum glucose levels in term neonates during the first 48 hours of life.
The Journal of Pediatrics 110, 119–122 (1987).
- Ho, H. T. Evaluation of ‘point of care’ devices in the measurement of low blood glucose in neonatal
practice.Archives of Disease in Childhood - Fetal and Neonatal Edition 89, F356–F359 (2004).
- Beardsall, K. Measurement of glucose levels in the newborn. Early Human Development 86, 263–
267 (2010).
- Committee on Fetus and Newborn. Postnatal Glucose Homeostasis in Late-Preterm and Term
Infants. PEDIATRICS 127, 575–579 (2011).
- Committee on Fetus and Newborn. Postnatal Glucose Homeostasis in Late-Preterm and Term
Infants. PEDIATRICS 127, 575–579 (2011).
- Thornton, P. S. et al. Recommendations from the Pediatric Endocrine Society for Evaluation and
Management of Persistent Hypoglycemia in Neonates, Infants, and Children. The Journal of
Pediatrics 167, 238–245 (2015).
- Williams, A. F. Hypoglycaemia of the newborn: Review of the literature. World Health Organization
(1997).