After completion of this chapter the participant should be able to:
Hypoglycaemia is common in LBW and very sick NYI and should always be considered early in management. 20% of infants below seven days of age have hypoglycaemia. It is important to identify hypoglycaemia as there is an increased association with convulsions, permanent brain injury, and mortality
COIN defines hypoglycaemia as blood glucose of < 45 mg/dl (2.5 mmol/L) for NYI. Blood glucose levels can be checked using a glucometer.
Newborns at risk of hypoglycaemia
Any baby who has:
Also:
Assessment of blood glucose with a glucometer should be conducted as part of routine assessment for all infants on admission.
Glucometers should also be used during continuing management for all sick or at-risk patients. Hypoglycaemia may present as:
Identify a NYI with Hypoglycaemia
Zoom in for details.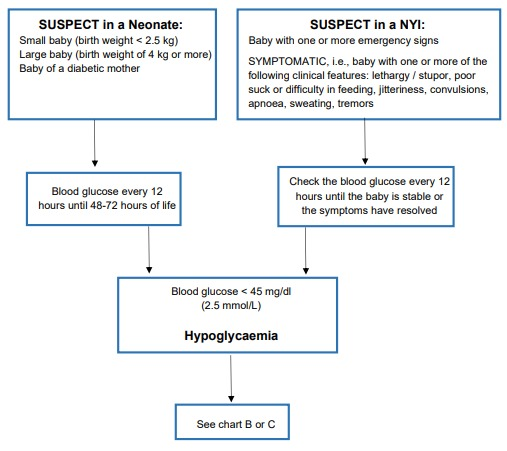
Management of a baby with blood glucose of less than < 45 mg/dl (2.5 mmol/l) and NOT symptomatic
Zoom in for details.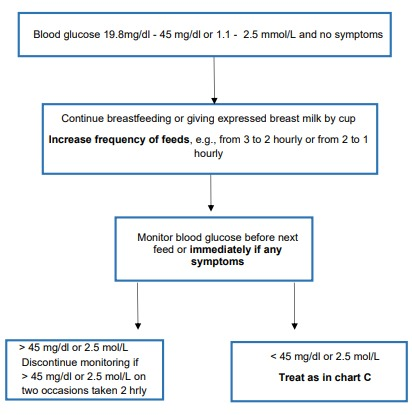
Management of a baby with blood glucose of less than < 45 mg/dl (2.5 mmol/l) and symptomatic
Zoom in for details.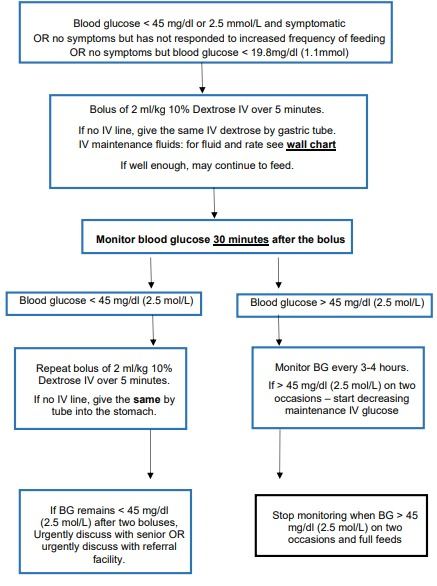
| Size | Water for Injection or Ringers Lactate or Normal Saline (4 parts) |
50% Dextrose (1 part) |
|---|---|---|
| 5 ml syringe | 4mls | 1ml |
| 10 ml syringe | 8mls | 2mls |
| 20 ml syringe | 16mls | 4mls |
| 50 ml syringe | 40mls | 10mls |
| 100 ml burette | 80mls | 20mls |
| 200 ml bag | 160mls | 40mls |
Empty fluid out of a litre bag of IV normal saline until there is only 200mls left (4 parts) and then add 50mls of 50% dextrose (1 part) to make up 250mls of a 10% dextrose solution.
| 250mls in a litre bag | 200mls of normal saline RL solution |
50mls of 50% glucose |
|---|
GIVING 50% GLUCOSE IS NO LONGER RECOMMENDED
After a bolus of glucose a plan must be made to continue providing a glucose supply as:
Neonatal hyperglycaemia is defined as a blood glucose of more than 145mg/dl (8mmol/L) regardless of body weight, gestational or postnatal age. Hyperglycaemia may be seen in any baby but is more common in low birth infants.
In settings where a neonate is on IV fluids the most common cause is infusion of inappropriately high amounts of glucose as IV fluids. In our setting, where IV infusions are less frequently given, hyperglycaemia is most commonly due to stress, usually from an intercurrent sickness such as sepsis, dehydration and HIE. This is because of raised cortisol levels in response to the stressful situation. Adequate treatment of the underlying illness will often result in resolution of the hyperglycaemia and improvement of baby’s overall condition. Rarely patients may have insulin resistance or neonatal insulin dependent diabetes mellitus and such patient need discussion and care at a tertiary level facility.
What should be done when a neonate has a high glucose reading?