After completion of this chapter the participant should be able to:
C represents Coma and Convulsion
in the ABCCCD system.
The following signs indicate impaired neurological status:
| Key Facts for Providers: How to Assess the NYI for Coma |
|
AVPU To help you assess the conscious level of a child, a simple scale (AVPU) is used: A Is the baby Alert? V Is the baby responding to Voice? P Is the baby responding to Pain? (rub the sternum) U The baby who is Unresponsive to voice (or being shaken) AND to pain is Unconscious. |
This assessment depends on your observation of the child and the history from the parent. Children who have a history of convulsion, but are alert and not currently convulsing, need a complete clinical history and investigation, but no emergency treatment for convulsions. Sometimes, in infants, the seizures are subtle, jerky movements may be absent, but there may be twitching (abnormal facial movements), apnoea, lip smacking, or abnormal movements of the eyes, hands or feet.
Among neonates with seizures, the reported causes and ranges of median prevalences are the following: hypoxic-ischaemic encephalopathy (HIE): 38-48%; hypoglycaemia: 3-7.5%; hypocalcaemia: 2.3-9%; central nervous system (CNS infections: 5.5-10.3% (7).
| Tetanus | Convulsions |
| Conscious | Unconscious |
| Increases with tactile stimulation, wind, light and noise | Does not change in response to stimulation |
Treatment of coma and convulsion are similar and will be described together.
To manage the airway of a convulsing child, gentle suction of secretions should be done, the infant put on his side, and oxygen started. Do not try to insert anything in the mouth to keep it open.
You have to observe the infant carefully
Initial Management of Coma and Convulsions
| Coma | Convulsion |
| Manage the airway | Manage the airway |
| Position the child | Position the child |
| Consider Guedel airway | Check the blood sugar |
| Check the blood sugar | Give IV glucose if low |
| Give IV glucose if low | Give anticonvulsant if still seizing |
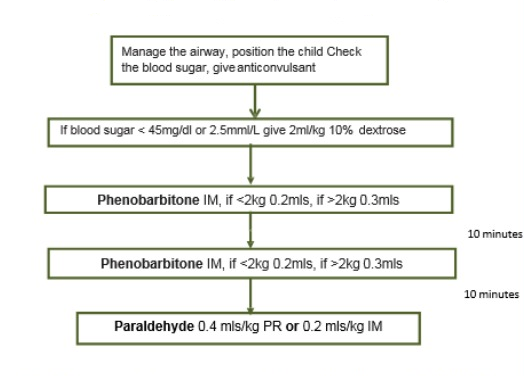
NB. The volumes in the chart above assumes that the phenobarbitone being used is of 200 mg/ml preparation. The dose is actually 20mg/kg and should be recalculated if the vial concentration is different.
NB. The volumes in the chart above assumes that the phenobarbitone being used is of 200 mg/ml preparation. The dose is actually 20 mg/kg and should be recalculated if the concentration is different.
Inj. Phenobarbitone intravenous dose (200 mg/ml) dose is 20 mg/kg.
| Weight of Infant | Initial Dose | Repeat Dose |
| 2 kg or less | 0.2 ml | 0.2 ml |
| 2 to 4 kg | 0.3 ml | 0.3 ml |
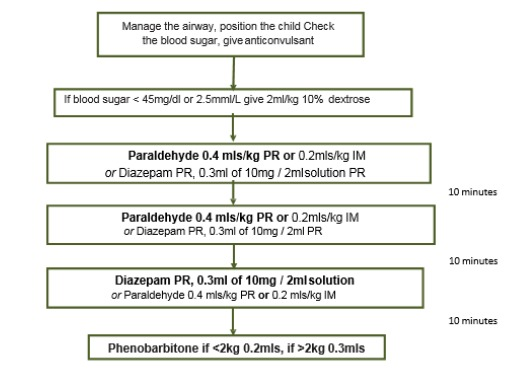
Or calculate as phenobarbitone loading dose 20 mg/kg IV. Phenobarbitone to be given IM and not IV.
| Age / Weight | Dose 0.1 ml/kg |
| 2 weeks to 2 months | (<4kg) 0.3ml |
Or calculate as rectal diazepam 0.4mg mg/kg/dose.
Diazepam may cause respiratory arrest – DO NOT GIVE IN BABIES <2 WEEKS.
| Age / Weight |
Dose: 0.2 ml/kg IM, 0.4 ml/kg PR; Injection 10 ml ampoules |
| 2 kg | 0.4 mls IM or 0.8 mls PR |
|---|---|
| 3 kg | 0.6 mls IM or 1.2 mls PR |
| 4 kg | mls IM or 1.6 mls PR |
Do not leave in plastic syringe for longer than 10-15 min and paraldehyde should not be given IV. All drug dose calculations must be carefully checked because drug ampoules may come in different strengths.
|
Key Facts for Providers: How to Assess and Manage the NYI for Coma and Convulsions |
|