Sepsis in NYI (Chapter 15)
Learning Objectives
After completion of this chapter the participant should be able to:
See investigations in case of suspicion of sepsis
See for assessment and management of meningitis
Risk factors for Sepsis
NYI have immature immune systems and have just been colonised with bacteria during their
recent delivery. They are therefore prone to infections which are likely to cross barriers, for
example between the lungs and blood, the gut and blood and meninges. Many NYI infections
can be prevented by good hygiene at the time of birth, early and exclusive
breastfeeding,
appropriate umbilical cord care, appropriate eye care, using
KMC and avoiding separation of
the mother and infant.
Common systemic bacterial infections in young infants include sepsis, pneumonia, urinary
tract infection, and meningitis and all these may present alike. Sepsis is a clinical syndrome
of systemic illness accompanied by septicaemia (bacteria in the blood). It is also called
bacteraemia.
Risk Factors for Sepsis and Clues to Infection
The risk factors for sepsis in the NYI are:
- Intrapartum maternal fever (temperature > 38oC)
- Membranes ruptured more than 18 hours before delivery
- Foul smelling or purulent amniotic fluid
- Untreated STI like syphilis
- Suspected or confirmed sepsis in twin
The babies born to mothers with these risk factors may be symptomatic or asymptomatic. Both
symptomatic and asymptomatic should be treated as having sepsis with IV antibiotics as the
risk for neonatal infection and the mortality rates are high.
Initial Assessment and Treatment of Sepsis in the NYI
ABCCCD
Assess ABCCD and manage the problems identified.
Provide supportive care and monitoring for the sick NYI.
Start empiric antibiotics; give penicillin and gentamicin – see doses in
wall charts.
Give (flu) cloxacillin
instead of penicillin if extensive skin pustules or abscesses are
present as these may indicate a staphylococcus infection.
Symptoms and Signs of sepsis in a NYI:
- Lethargy, decreased movement
- Axillary temperature 37.5oC or above (or feels hot to touch) or temperature < 35.50C
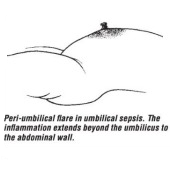
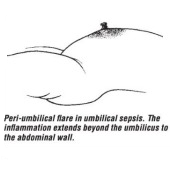
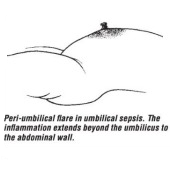
- Umbilical redness extending to the periumbilical skin or umbilicus draining pus,
skin pustules, big boil (abscess).
- Painful joint/swelling, reduced movement
and irritability if these parts are handled.
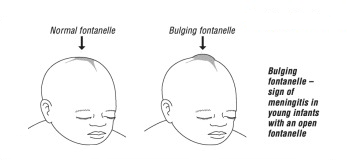
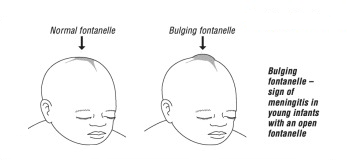
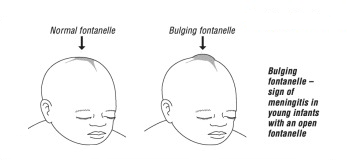
- Bulging fontanelle
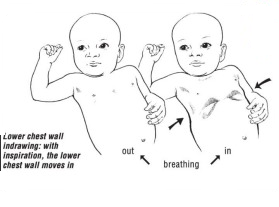
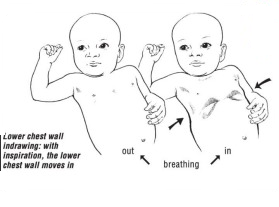
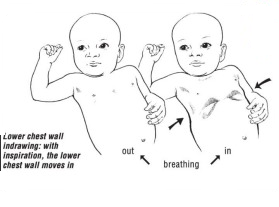
- Grunting, nasal flaring, fast breathing, chest in drawing,
crepitation’s in the lungs.
Look for these risk factors and do a septic screen. If the sepsis screen is negative and the
infant remains asymptomatic, antibiotics may be discontinued after five days.
Investigations
A sepsis screen should be done in such infants before IV antibiotics:
- WBC (< 5000 or > 20,000 cells/µl are very likely sepsis in age > 72 hrs).
- Lumbar puncture.
- Blood culture.
- Urine culture.
Empiric antibiotic therapy and dose for sepsis:
Note: If a baby develops a fever after being in the neonatal unit for >72hrs it is likely to be a
hospital acquired infection. These infections need treatment with the addition of ceftriaxone.
If less than 72 hours Benzyl penicillin in combination with Gentamicin are the drugs of choice.
| ANTIBIOTIC |
EACH DOSE |
FREQUENCY |
ROUTE |
| Age < 7 days |
Age > 7 days |
Benzyl
penicillin |
50,000 IU/kg |
12 hrly. |
6 hrly. |
IV, IM |
| AND |
| Gentamicin |
LBW:
3 mg/kg
Term:
5 mg/kg
>7 days:
7,5 mg/kg |
24 hrly. |
24 hrly.
(7,5 mg/kg/dose) |
IV, IM |
| |
Ceftriaxone
[2nd line drug]
|
50-100 mg/kg |
24 hrly. |
24 hrly. |
IV |
| If Benzyl penicillin is not available, Ampicillin or (Fluc)cloxacilin can be used as an
alternative
|
| Inj. Ampicillin |
25 mg/kg |
<2kg: 12hrly |
<1.2kg: 12hrly
1.2-2kg: 8 hrly. |
IV/IM |
| >2kg: 8hrly
|
>2kg: 6hrly |
IV/IM |
| (Flu)Cloxacillin |
50 mg/kg |
12 hrly. |
6 hrly. |
IV |
Key Facts for Providers:
Supportive Care for NYI with Sepsis |
- Ensure warmth.
- Gentle stimulation if apnoeic, consider aminophylline if premature and current
age is estimated to be < 37 weeks gestation.
- Respiratory support with oxygen or CPAP if there is severe respiratory distress
or apnoea.
- If shocked treat according to the impaired circulation protocol.
- If hypoglycaemic, infuse 2mls/kg of 10% dextrose stat and recheck in 30 minutes,
continue maintenance 10% dextrose.
- If they have not received Vitamin K, give 1mg intramuscularly as septic NYI may
have an increased tendency to bleed.
- If very sick, e.g., continuous convulsions, avoid oral feeds, give
maintenance fluids.
Treat convulsions
if present.
- Treat jaundice if present with phototherapy
|
Key Facts for Providers:
Empiric Antibiotics and Duration |
- Empiric antibiotics means that the organism causing the sepsis has not yet been
identified and the antibiotics selected will treat the organisms most likely to cause
this presentation in this age group.
- If there is no blood culture or the blood culture is negative and even if the baby is
well, continue to treat with the empiric antibiotics for a minimum of 5 days.
- If the baby was clinically septic - treat for 7-10 days (except meningitis and
bone/joint infection which will require longer duration antibiotics).
- If not improving in 48 hours the antibiotic treatment may need to be changed from
the first line (penicillin and gentamicin) to second line, which is often ceftriaxone
but this depends where you work).
|
How to Prevent Sepsis in a NYI
- Ensure early and exclusive
breast feeding
- Practice rooming-in 24/7 for healthy newborn.
- Kangoroo Mother Care
in premature babies.
- Good hand hygiene at all times for medical and nursing staff and visitors.
- Check HIV
and VDRL status of mother and start treatment in neonate where
necessary.
- Keep baby normothermic at all times.
- Remove IV cannulas as quickly as possible.